Our Healthcare System emphasizes care coordination of clinical activities as a way to improve outcomes and lower costs. There is a lot of discussion around Accountable Care Organizations and longitudinal health records especially when it comes to chronic illness. Does care coordination in the clinical space act as the primary driver for better outcomes and lower cost? Or is it an outcome of effective healthcare communication? I believe that effective two- way health communications at all touch points in a healthcare encounter are the real path to solving our cost and outcome issues in the healthcare industry.
The National Institutes of Health definition for health communication is as follows:
Health Communication: The study and use of communication strategies to inform and influence individual and community decisions that enhance health
What are two way communications?
Two-way communications start by providing the critical information to the patient in a format that accommodates any barriers in language, education and culture. These communications then seek to gather and confirm all patient information that will increase the accuracy of the patient profile. Improving the accuracy of patient data can help reduce barriers in language, education and culture and refine the clinical approach to treatment. Currently, the vast majority of healthcare communication touchpoints fail to do this.
The following graphic highlights the wide variety of communication touch points that potentially exist in a healthcare encounter.
Communication touch points in Healthcare
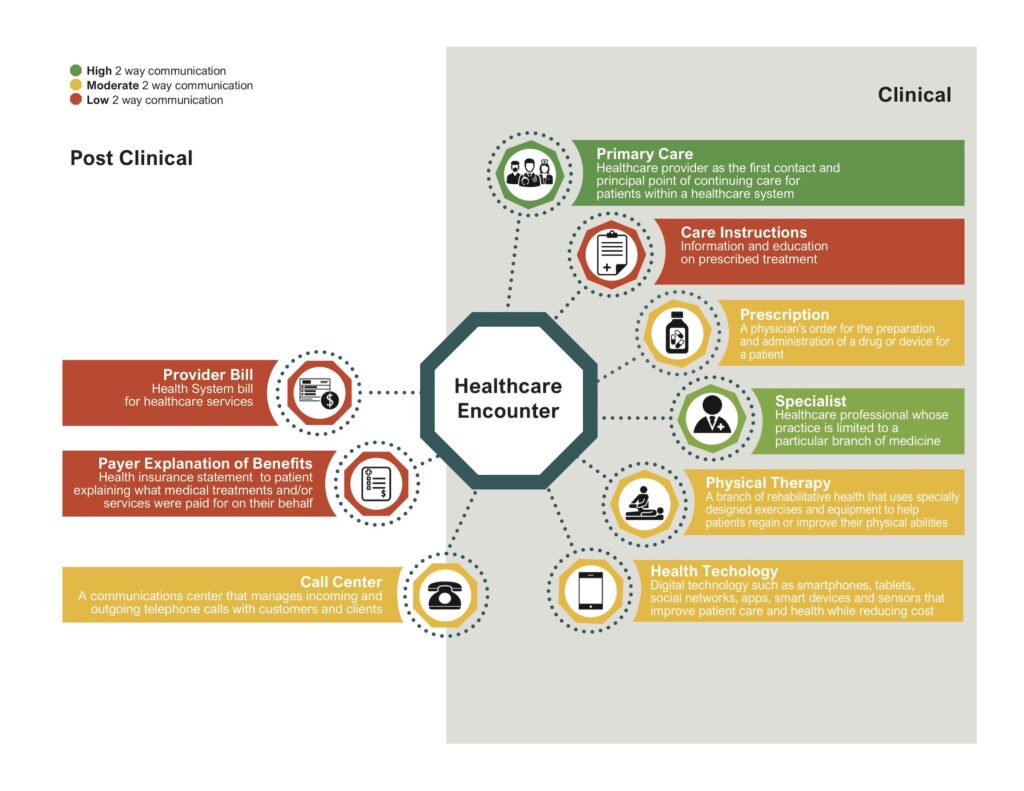
The reality is that healthcare encounters generate communication touchpoints in BOTH clinical and non-clinical environments. Yet we keep focus only on the clinical and lose sight of the potential value of EVERY touchpoint. The disparate nature and conflicting approach to each of these touchpoints cause confusion and inefficiency.
With this in mind, how do each of these healthcare encounter touchpoints work?
- Green Items: Face to face communications with your Primary Care Doctor and Specialists represent the main two-way communication that sets and adjusts a clinical course of action. They are affected by the communication skills of the doctor and any patient-related barriers like language, education or culture.
- Yellow Items: (Prescription, Physical Therapy, Health Technology and Call Center) These have the potential for two-way communication but are still predominately push oriented. That is, they provide information to the patient with the hope that they take the time to understand and act upon it. Even if they are set up to gather information they may not be very effective.
- Red Items: (Care Instructions, EOB, Provider Bill) Primarily push communications that hope to stimulate some form of action or adherence. Little to no information gathering.
How many of the healthcare encounter touchpoints shown above currently represent an opportunity for two-way communication? The short answer is very few. Even if they have the ability to capture feedback most are still push oriented.
Do patients want two way communications?
The CDC published a presentation which documented a wide variety of recommendations on improving medication adherence in the treatment of chronic illness. One of the key elements is called bidirectional communications:

This is an important point. Not only do patients want bidirectional communications, but they also want to be an active participant in the development of their treatment plan.
Accountable Care or Accountable Communications?
The accuracy and depth of healthcare patient data is critical in deciding on treatment and creating effective health communications that stimulate action. Every missed opportunity to expand and deepen the patient relationship, to refine the accuracy of your patient profile, and to increase patient health literacy undermines the goal of lower costs and better outcomes.
We want to coordinate care in the clinical space, but our focus should be expanded to include coordinating care AND coordinating two-way communications across all touchpoints in every healthcare encounter, especially when dealing with chronic illness. We want to create a longitudinal health record, how about a longitudinal communication strategy? Working both of these areas concurrently will provide us the real opportunity to change healthcare.
Where might two-way communications make the most difference?
We have a goal of coordinating care but how might we coordinate two-way communications?
Start with the most expensive patients in healthcare: Individuals with multiple chronic conditions. There are two reasons for this. First, most healthcare encounters don’t need it. The patient has an issue, they visit the doctor, a solution is recommended, and the patient moves back to full health. You have effective two-way communication that captures the interaction because there is typically one visit and the healthcare issue is resolved.
Chronic illness is very different. The issues are typically long term and the costs of non-conformance are very high. Study after study documents how patients with multiple chronic conditions generate the majority of healthcare expense in the United States. This segment is also the focus of technology vendors with platform-based population health solutions that target specific chronic illness like diabetes, hypertension, heart disease and more. There is considerable investment in this space.
For chronic-illness groups we would create communications across all the touchpoints generated in the healthcare encounter and they would have the following characteristics.
- Two-way communications: Every single touchpoint on the graphic would be enabled to push data out AND pull data back in from the patient. Communications would use persuasion research to stimulate action. Every message would provide links, application, or phone-based connections that seek to validate existing information and gather new information.
- Data Sharing: This is a patient’s longitudinal communication record. All captured feedback that adds value to the health record AND future communications would be shared across their healthcare providers and payer. This is important when trying to address barriers in language, education or culture that inhibit the patient’s ability to manage their chronic illness.
- Message Coordination: If you message patients with diabetes it would make sense that every communication touchpoint in the graphic reinforces the same core recommendations no matter who sends the communication. This would also ensure that patient preferences in communication format and delivery are the same across their disparate healthcare interactions.
There is no simple answer to this, especially given the huge growth in population-health platforms and the growing use of technology as part of healthcare. The key will be finding a balance between the potential lower cost/better outcomes and the investment/coordination required to truly implement accountable communications across all touchpoints. This blog will focus on all the different variables at play here with the hope to stimulate discussion on how we can move to a future that coordinates care AND communications as a way to generate better outcomes and lower costs for chronically ill patient populations.
I encourage you to share your thoughts in the comment section.

No Comments